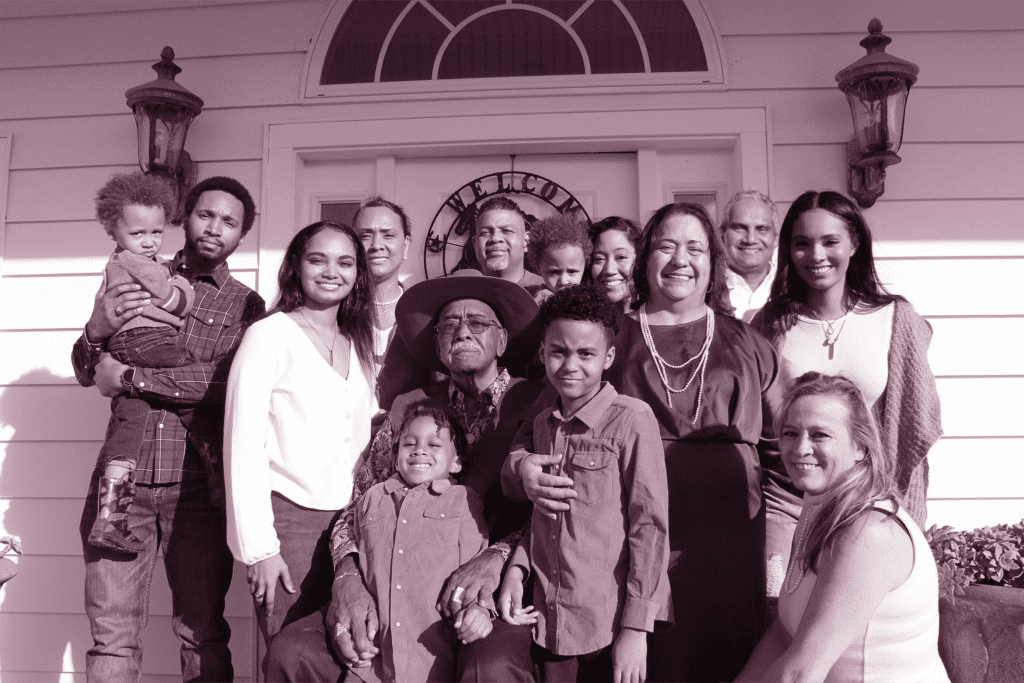
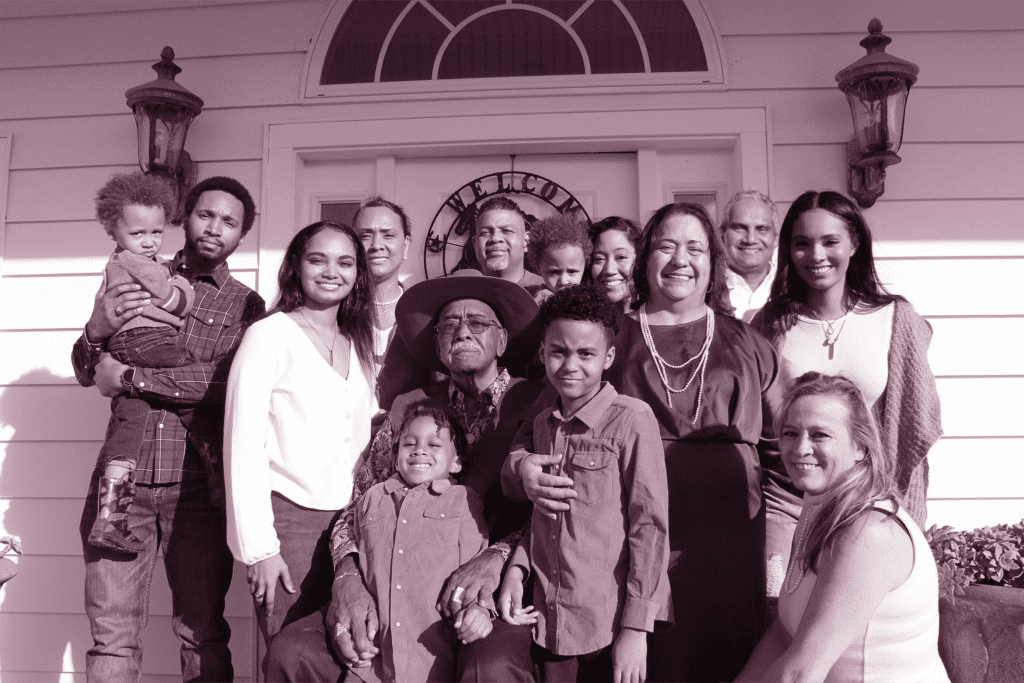
Dr. Gorman’s unwavering commitment to delivering unmatched and customized healthcare consistently leads the way in comprehending the complex nature of breast cancer. Our primary goal at Texas Breast Center is to foster an informed community, one that is equipped with the knowledge needed to prevent, detect, and address breast cancer efficiently. It’s with this vision that we delve into the topic of “Breast Cancer Causes: Age Related Risks.”
Breast cancer is a complex disease with a myriad of contributing factors. Among these, age stands as a significant determinant. Despite the prevalence of breast cancer in younger women, it’s important to note that the risk indeed increases as women get older.
In this article, we’ll explore the reasons why age is a risk factor, the mechanisms behind this link, and provide practical advice on how women of all ages can monitor their breast health effectively.
This article embodies Dr. Gorman’s commitment to offering an advanced and targeted approach to breast health. Our aim is not just to treat but to educate, empower, and encourage women to take an active role in their health journey. Our hope is that through this understanding, we can collectively reduce the impact of breast cancer and improve the lives of women across Texas and beyond.
We invite you to take this journey with us, one step at a time, toward a future where knowledge and proactive actions make a significant difference in the fight against breast cancer.
Increasing age
Breast cancer risk is intrinsically linked with age, with an increased probability of developing the disease as women get older. This is primarily due to the cumulative effect of several risk factors over time, including exposure to estrogen, genetic mutations, and the natural wear and tear process at the cellular level.
Estrogen exposure plays a significant role in breast cancer risk. This hormone is necessary for normal breast development, but it can also facilitate the growth of some types of breast cancer. Throughout a woman’s life, her body is exposed to varying levels of estrogen, primarily produced by the ovaries. Women who have had longer menstrual histories (i.e., those who started menstruating early and/or went through menopause late) have a slightly higher risk due to longer lifetime exposure to the hormone.
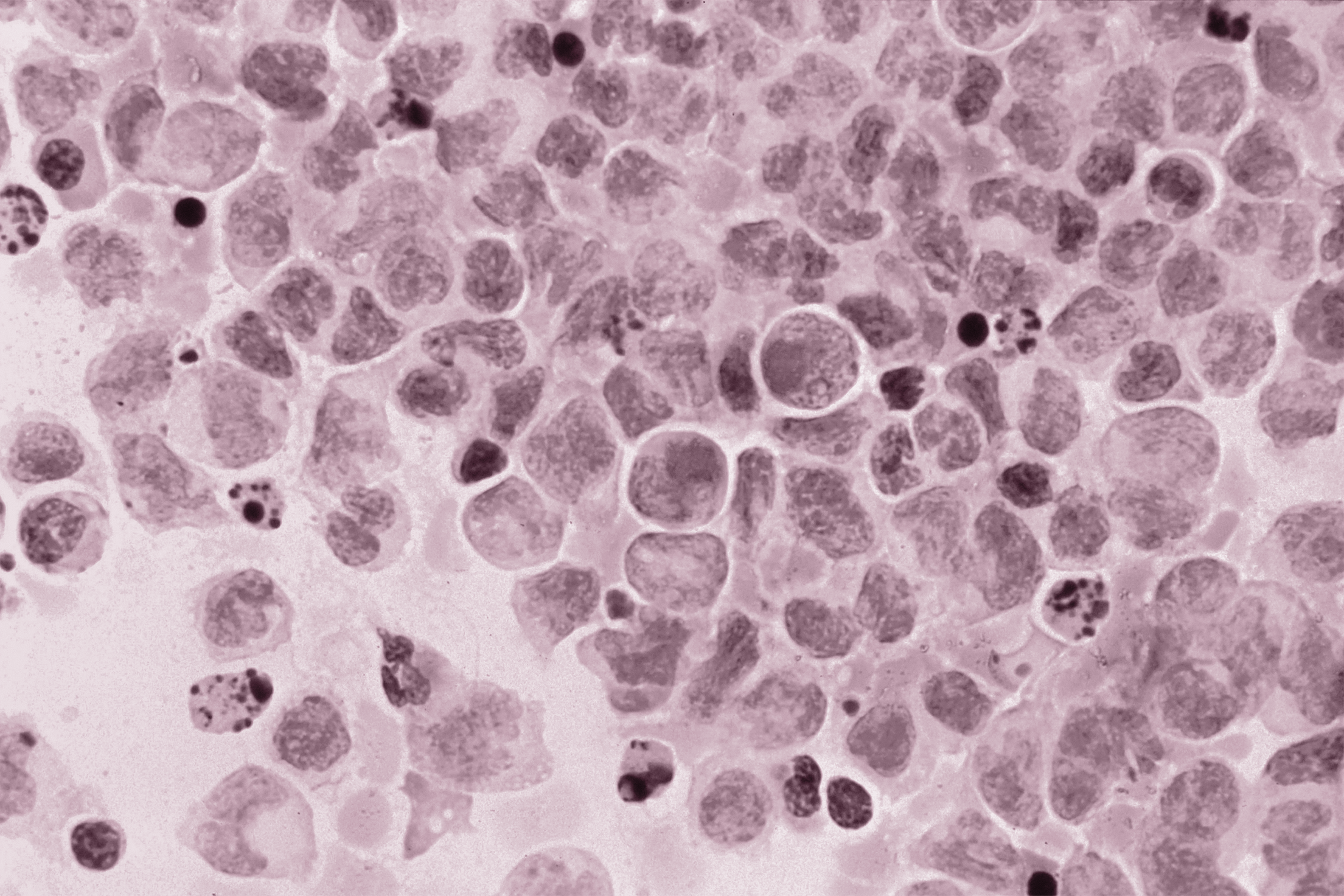
With increasing age, the likelihood of genetic mutations also increases. These mutations can accumulate over time due to various factors such as exposure to radiation, certain chemicals, and random errors that occur when cells divide. Some of these mutations can cause cells to become cancerous.
Moreover, the aging process naturally brings about a decline in the body’s immune function, reducing its ability to detect and destroy cells that have become abnormal, potentially leading to cancer.
While breast cancer can and does occur in younger women, it is less common. According to the American Cancer Society, the average risk of a woman developing breast cancer increases dramatically with age. Statistically, the majority of breast cancer cases are diagnosed in women over the age of 50. In fact, the median age for breast cancer diagnosis in the United States is 62, with most cases occurring in this age bracket. This is not to say that younger women should not be vigilant; rather, it underscores the importance of regular screenings, especially as women age.
Younger women
Breast cancer is relatively rare in younger women, with very few breast cancer cases in the U.S. being diagnosed in women under the age of 40, according to the American Cancer Society. This is due to several reasons, one being that breast tissue in younger women is denser, which may limit the effectiveness of mammography and lead to later detection. Moreover, younger women have fewer cumulative lifetime exposure to various risk factors like estrogen.
However, when breast cancer does occur in younger women, it tends to be diagnosed at a later stage and often presents as more aggressive forms of the disease. One reason for this is that breast cancer in younger women can be more difficult to detect due to the dense breast tissue, as mentioned before. This might delay diagnosis and consequently, treatment.
Moreover, younger women are more likely to have what is known as “triple-negative” breast cancer – a type of breast cancer that is particularly aggressive and less responsive to standard hormonal therapies. This subtype of cancer does not express the three most common types of receptors known to fuel breast cancer growth—estrogen, progesterone, and the HER-2/neu gene. Therefore, treatment options can be more limited and the cancer can be more challenging to treat successfully.
Another aggressive form that occurs more commonly in younger women is HER2-positive breast cancer, which is characterized by the overexpression of the HER2 protein. This form of breast cancer tends to grow and spread more quickly than other types.
It’s important to note that, regardless of age, any new or unexplained breast symptoms should be evaluated promptly by a healthcare professional. For younger women, especially those with a family history of breast cancer or other risk factors, proactive measures such as self-examinations, regular clinical exams, and discussions with healthcare providers about individual risk can contribute significantly to early detection and improved outcomes.
Age at first menstruation
The age at which a woman starts menstruating, also known as menarche, can indeed influence her risk of developing breast cancer later in life. Research indicates that women who experience their first period before the age of 12 have a slightly elevated risk of developing breast cancer compared to those who started menstruating at a later age.
This association primarily stems from the lengthened exposure to estrogen and progesterone – hormones that are known to stimulate breast cell growth. Simply put, the earlier a girl starts her periods, the longer her lifetime exposure to these hormones.
During each menstrual cycle, the levels of estrogen and progesterone in a woman’s body rise to prepare for a potential pregnancy. These hormonal surges stimulate the growth of the glandular tissue in the breasts. Although this is a natural process, over time, this increased cell activity raises the chances of a DNA error during cell division, potentially leading to cancerous mutations.
In addition, early menstruation usually means a longer time until menopause. Menopause is another significant event in a woman’s life when the ovaries stop producing eggs, and the production of estrogen and progesterone declines. Therefore, the longer time from menarche to menopause translates into more menstrual cycles, and subsequently, a longer cumulative exposure to estrogen and progesterone.
While the increased risk linked with early menarche is relatively small on an individual level, it’s significant from a public health perspective given the high prevalence of breast cancer. This connection underlines the importance of regular breast cancer screenings, especially for women who began menstruating at an early age.
Age at menopause
The age at which a woman reaches menopause also significantly influences her risk of developing breast cancer. Research suggests that women who experience menopause after the age of 55 have a slightly increased risk of breast cancer compared to women who reach menopause before the age of 45.
This heightened risk is predominantly due to prolonged exposure to hormones such as estrogen and progesterone, which are produced in a woman’s body during her reproductive years. These hormones have been associated with stimulating cell growth in the breasts, and prolonged exposure to them can increase the chance of DNA errors during cell division, which can result in cancerous mutations.
Late menopause means that a woman’s body continues to produce these hormones, and her breast tissue continues to be exposed to their growth-promoting effects for a longer duration. This cumulative hormonal exposure over many years increases the likelihood of developing breast cancer.
Moreover, the risk associated with late menopause might also be linked to the increased number of menstrual cycles a woman goes through in her lifetime. Each menstrual cycle is associated with a surge in estrogen and progesterone levels, which stimulate breast cell multiplication, potentially leading to errors in cell replication and an increased risk of mutation.
While the increased risk associated with late menopause is considered modest, it’s significant enough to warrant attention, especially considering the high incidence of breast cancer. Therefore, it is crucial for women who experience late menopause to engage in regular screenings and take proactive steps to reduce their breast cancer risk. These steps can include maintaining a healthy lifestyle, which involves regular physical activity, a balanced diet, limiting alcohol consumption, and avoiding tobacco.
Age at first full-term pregnancy
The age at which a woman has her first full-term pregnancy can influence her risk of developing breast cancer. Research has shown that women who have their first full-term pregnancy after the age of 30 have a slightly increased risk of developing breast cancer compared to women who have their first child before the age of 20.
This somewhat counterintuitive relationship between pregnancy and breast cancer risk is likely due to the complex interplay of hormonal changes that occur during pregnancy. Pregnancy induces significant changes in the levels of hormones such as estrogen and progesterone in a woman’s body, and these hormones have a profound impact on the cells of the breast.
During a first full-term pregnancy, the breasts undergo permanent cellular changes. Before this, the breast cells are immature and more susceptible to the carcinogenic effects of hormones and environmental toxins. A full-term pregnancy matures these cells, making them less likely to become cancerous.
However, this protective effect is more pronounced when the first full-term pregnancy occurs at a younger age. When the first full-term pregnancy occurs after the age of 30, the breast cells have had more time to accumulate genetic damage, which could potentially lead to cancer. Thus, the overall effect of a later first pregnancy might result in a net increase in breast cancer risk.
Moreover, during pregnancy, especially in the early stages, levels of estrogen increase, which leads to rapid growth of breast cells. This increased cell division can raise the risk of mutations and cancer development.
Despite this slight increase in risk, it’s important to note that the decision to have children and when to have them is personal and can be influenced by various factors. It’s just one of many factors that contribute to breast cancer risk, and having a first child after 30 does not guarantee one will develop breast cancer. As always, regular screenings and healthy lifestyle choices are key components in the proactive management of breast cancer risk.
Age at first childbirth
The age of a woman at the time of her first childbirth, or not having given birth at all, can influence her risk of developing breast cancer. Research indicates that women who never have a full-term pregnancy have a slightly higher risk of breast cancer compared to those who have their first child at a younger age.
One of the primary reasons behind this increased risk is the prolonged and uninterrupted exposure to estrogen and progesterone. These hormones are naturally produced during a woman’s menstrual cycle and have been associated with increased cell growth in the breasts. A woman who has never been pregnant has more menstrual cycles compared to a woman who has one or more pregnancies, thus increasing her cumulative lifetime exposure to these hormones.
During pregnancy, the breasts go through changes that make them more resistant to transformations that can lead to cancer. The cells of the breast differentiate, or specialize, to produce milk – a change that seems to make the breast cells less likely to undergo cancerous changes. An absent pregnancy means the breast tissue goes through fewer of these protective changes.
Additionally, the surge of hormones during pregnancy causes breast cells to rapidly divide and grow. While this is normal, increased cell division can also increase the chance of genetic mistakes or mutations, potentially leading to cancer. The risk of this occurring is higher in older women, as cells accumulate genetic changes over time.
It’s crucial to note that while these factors do contribute to an increased risk, it’s a relative increase and the overall risk remains modest. Not having children is a personal decision influenced by a wide range of factors. Regular breast cancer screenings and maintaining a healthy lifestyle remain the most effective strategies for all women to manage their individual risk.
Age at breast cancer diagnosis
While it’s true that breast cancer risk increases with age, the nature of the disease can vary based on the age at diagnosis. Generally, older women (especially those over 70) diagnosed with breast cancer tend to have a more favorable prognosis compared to younger women. This is, in part, due to the fact that breast cancers in older women often grow more slowly.
Cancer growth rate is significantly influenced by the characteristics of the cancer cells and the surrounding environment. Age-related changes in both the breast tissue and the body’s overall immune response can impact the rate at which a tumor grows.
Breast cancers in older women are often hormone receptor-positive, meaning that the cancer cells have receptors that attach to hormones like estrogen and progesterone. Hormone receptor-positive cancers tend to grow more slowly than cancers that are hormone receptor-negative. Moreover, treatments that block these hormones or their receptors can effectively slow or stop the growth of these cancers.
Furthermore, older adults often have a reduced immune response, which paradoxically, may slow the growth rate of the cancer. An aggressive immune response can sometimes stimulate cancer cells to grow and divide more rapidly, a phenomenon known as inflammation-induced tumor growth. The diminished immune response in older adults may limit this effect.
However, it’s important to note that although the prognosis may be generally better due to slower tumor growth, older women might face other challenges related to breast cancer management. These can include an increased risk of treatment side effects and the presence of other health conditions that might complicate care. Therefore, an individualized and comprehensive approach to treatment is crucial.
Finally, regardless of age, early detection remains the key to a more favorable prognosis in breast cancer. Regular screenings and understanding personal risk factors contribute significantly to early diagnosis and effective treatment.
Age-specific breast cancer rates
Breast cancer incidence rates do indeed vary by age group. It’s a well-established fact that the risk of developing breast cancer increases as women age. According to the American Cancer Society, women aged 70-74 generally have the highest incidence rates of breast cancer.
This trend can be attributed to several reasons. First, the process of aging itself results in an accumulation of genetic mutations over time due to factors like exposure to carcinogens, errors during DNA replication, and decreased efficiency of DNA repair mechanisms. These factors can eventually lead to the development of cancer.
Second, older women have had more menstrual cycles, resulting in a longer lifetime exposure to hormones such as estrogen and progesterone. These hormones, which are known to stimulate cell growth in the breasts, can over time lead to uncontrolled cell growth and potential transformation into cancer cells.
Third, as women age, they experience more instances of proliferative breast diseases with atypia, which are known risk factors for breast cancer. Atypia refers to the presence of abnormal cells, which are more likely to become cancerous.
Furthermore, the body’s immune system, which helps to detect and destroy abnormal cells, declines with age. This decline might allow some cancerous cells to multiply and form tumors before they’re detected by the immune system.
Despite the higher incidence rate in older women, it’s important to note that breast cancer can occur at any age, and younger women can also develop aggressive forms of the disease. Therefore, it’s crucial for women of all ages to understand their individual risk factors, including genetics, and engage in recommended screening practices for early detection of the disease. It’s also essential to maintain a healthy lifestyle, as several risk factors for breast cancer, such as maintaining a healthy weight and regular physical activity, are within an individual’s control.
Age-related hormone exposure
Estrogen and progesterone are hormones that are naturally produced in a woman’s body and play crucial roles in the menstrual cycle and pregnancy. However, longer lifetime exposure to these hormones has been associated with an increased risk of developing breast cancer.
This increased risk is predominantly due to the role these hormones play in cell growth. Both estrogen and progesterone stimulate the growth of cells in the breast — a normal process that facilitates the development and maintenance of the mammary glands in response to each menstrual cycle. However, with longer exposure to these hormones, there is an increased opportunity for the growth of cells in the breast. This increased cell division can potentially result in errors during the replication of DNA, which can, in turn cause mutations that may lead to cancer.
In essence, the longer the breast tissue is exposed to these hormones, the higher the chance that a breast cell could turn cancerous. Factors that can lengthen a woman’s exposure to these hormones include early menarche (starting menstruation before age 12), late menopause (experiencing menopause after age 55), late or no pregnancy, and certain types of hormone replacement therapy or birth control. Each of these conditions leads to a longer timeframe during which the breast tissue is exposed to estrogen and progesterone, thereby increasing the risk of breast cancer.
It’s also worth noting that not all breast cancers are hormone receptor-positive, meaning that not all breast cancers grow in response to estrogen or progesterone. Some types of breast cancer are hormone receptor-negative and grow independently of these hormones. Therefore, while it’s true that longer lifetime exposure to estrogen and progesterone increases the risk of breast cancer, it’s not the only factor at play.
Nevertheless, understanding this relationship underlines the importance of regular breast cancer screenings and lifestyle modifications where possible, to manage and mitigate the risk associated with prolonged hormone exposure.
Age and breast cancer screening
Mammograms, which are X-ray images of the breast, are an essential tool for the early detection of breast cancer. Regular mammogram screenings are typically recommended for women aged 40 and older, though the exact age to start and frequency of screenings can depend on individual risk factors and professional guidelines.
The primary aim of a mammogram screening is to identify breast cancer before any physical symptoms develop. Detecting cancer at an early stage often means that it is smaller and hasn’t spread, which makes it easier to treat successfully. The five-year relative survival rate for women with localized breast cancer (cancer that has not spread outside the breast) is nearly 99%.
A mammogram can identify changes in the breast up to two years before a patient or physician can feel them. Regular screenings can help catch the disease in its earliest stages, when it’s most treatable. This not only improves a woman’s chance of recovery but also offers more treatment options.
For example, women diagnosed with early-stage breast cancer might be candidates for breast-conserving surgery, such as lumpectomy, which involves removing the cancer and a small portion of healthy tissue around it but not the entire breast.
Moreover, early detection might also reduce the need for more aggressive treatments like chemotherapy. This can significantly lessen the physical and emotional impact of cancer treatment and improve quality of life for patients.
However, it’s essential to balance the benefits of mammograms with the potential harms, which can include false positives, over-diagnosis, and exposure to radiation. Each woman’s risk factors should be considered in decision-making about when to begin mammograms and how often to have them.
Lastly, while mammograms are a valuable tool, they are not perfect and do not detect all breast cancers. Thus, it’s crucial for women to understand and recognize any changes in their breasts and to have any changes evaluated by a healthcare professional. Awareness and early detection are key to the effective management of breast cancer.
Take Control of Your Breast Health – Schedule a Consultation with Dr. Gorman at Texas Breast Center Today
Navigating the complexities of breast cancer, its age-related risks, and the nuances of its potential causes can be challenging. That’s why Dr. Gorman and her team at Texas Breast Center are committed to offering you an advanced, personalized, and targeted approach to understanding and treating this disease. Their goal is to arm you with the knowledge you need to make informed decisions about your health and provide you with state-of-the-art care every step of the way. With a keen understanding that each patient’s journey is unique, Dr. Gorman is here to guide you through every stage of your care with empathy, expertise, and a relentless pursuit of the best outcomes possible.
Now, more than ever, it is vital for women of all ages to understand their personal risk factors for breast cancer and to engage in regular screenings. Remember, early detection is key to improving breast cancer prognosis and treatment options. We encourage you to discuss these risk factors and your personal history with a healthcare provider, like Dr. Gorman, who can help guide you through the process. Contact the Texas Breast Center today to set up an appointment for a consultation or to learn more about the services we provide. Together, we can face the challenges of breast cancer head-on and work towards a healthier, cancer-free future.
Read the other articles in the Causes series including Gender Influencing Causes.
Also, read the article about Treating Breast Cancer in Older Adults.
FAQ’s about Breast Cancer Causes: Age Related Risks
How much does breast cancer risk increase with age?
The risk of developing breast cancer approximately doubles every 10 years until menopause, after which the rate of increase slows. It’s estimated that around two-thirds of invasive breast cancers are found in women aged 55 or older.
Why does age increase the risk of cancer?
Age is a significant risk factor for cancer primarily due to the accumulation of genetic mutations over time and the body’s declining efficiency in repairing damaged DNA. Additionally, the immune system’s ability to detect and destroy abnormal cells decreases with age.
Why is breast cancer more common after 50?
Breast cancer is more common after 50 mainly because of the prolonged exposure to estrogen and progesterone, hormones known to stimulate cell growth in the breasts. Additionally, genetic mutations accumulate over time, increasing the likelihood of cancer development.
What is the highest age risk for breast cancer?
Breast cancer risk increases with age, with the highest incidence rates observed in women aged 70-74. However, the risk continues to be significant as women age beyond this.
Does age affect cancer survival rate?
Yes, age can affect cancer survival rates. Younger patients often have a better prognosis due to generally being healthier and better able to tolerate treatments. However, breast cancers in older women often grow more slowly and are hormone receptor-positive, which can lead to effective treatment options.
Why is breast cancer more common with age?
Breast cancer becomes more common with age due to a combination of factors such as lifetime exposure to estrogen and progesterone, the natural aging process leading to an accumulation of genetic mutations, and a decrease in the immune system’s ability to prevent the development of cancer.
Can you live 30 years after breast cancer?
Yes, it’s possible to live 30 years or more after a breast cancer diagnosis. Thanks to advancements in early detection and treatment, many women are living long, healthy lives following their diagnosis. The prognosis depends on many factors, including the cancer stage and type, the woman’s overall health, and the treatments used.
Is alcohol linked to breast cancer?
Yes, research consistently shows that drinking alcohol increases the risk of breast cancer. Even moderate consumption of an alcoholic beverage can increase breast cancer risk, and the risk increases the more alcohol is consumed.
Is breast cancer less aggressive in elderly?
Breast cancer in older women tends to be less aggressive and more responsive to hormone therapy than in younger women. This is mainly because most breast cancers in older women are hormone receptor-positive. However, diagnosis can be complicated by the presence of other age-related health conditions.
https://www.cancer.org/cancer/types/breast-cancer/about/how-common-is-breast-cancer.html



 Late in 2017, the media picked up on a
Late in 2017, the media picked up on a