Breast cancer remains one of the most commonly diagnosed cancers worldwide, making understanding its causes, particularly those related to lifestyle, incredibly important. Despite advancements in cancer research, prevention, and care, many are unaware of the significant role that lifestyle choices, such as diet, exercise, and alcohol consumption, play in the development of this disease. Dr. Gorman of Texas Breast Center is deeply committed to providing her patients with an advanced, personalized, and targeted approach to breast surgery and the treatment of breast cancer. Recognizing the importance of a comprehensive approach to cancer prevention and care, this article will delve into the many lifestyle risks associated with breast cancer.
Dr. Gorman and Texas Breast Center team understand that an essential aspect of breast health involves educating patients about the various lifestyle factors that can influence their risk of developing breast cancer. It is crucial to understand the connection between lifestyle choices and breast cancer risk to implement necessary lifestyle changes and engage in cancer-preventive behaviors. This article aims to provide a thorough examination of the relationship between lifestyle risks and breast cancer. By exploring these topics, this article hopes to empower individuals with the information needed to take proactive steps toward reducing their risk of breast cancer and promoting breast health.

Alcohol Consumption
Increased alcohol consumption is a significant lifestyle risk factor for breast cancer, with even small amounts raising estrogen levels and thereby increasing the risk. The American Cancer Society advises limiting alcohol to one drink per day, though some, especially those with a family history of breast cancer, may choose to abstain entirely. The type of alcohol consumed may also impact risk, with higher alcohol content beverages, like hard liquor, potentially posing a higher risk than beer or wine.
Dr. Gorman and her team at Texas Breast Center emphasize the importance of understanding the risks associated with alcohol consumption and breast cancer. They provide personalized recommendations for managing alcohol intake as part of a comprehensive approach to reducing breast cancer risk and optimizing overall health.
Physical Inactivity
Physical inactivity significantly increases breast cancer risk, and maintaining regular physical activity can regulate hormone levels associated with breast cancer development. Regular exercise and physical activity are vital for reducing breast cancer risk by maintaining healthy body weight and regulating hormone levels. Dr. Gorman at Texas Breast Center encourages regular exercise, aligning with the American Cancer Society’s recommendation of at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity exercise per week as part of a comprehensive approach to breast health and cancer prevention. Starting slowly and consulting healthcare professionals like Dr. Gorman before beginning a new regimen is essential, especially for those with existing health conditions or a higher breast cancer risk. They encourage patients to enjoy physical activities regularly, benefiting not only breast cancer prevention but also overall health by reducing the risk of other cancers, heart disease, stroke, osteoporosis, managing stress, and improving mood. In summary, regular physical activity reduces breast cancer risk and has multiple health benefits, and Dr. Gorman’s team is dedicated to helping patients incorporate it into their daily routine to improve overall health and well-being.
Diet
A balanced, nutritious diet is vital for reducing breast cancer risk. High-fat diets, processed foods, and low intake of fruits and vegetables contribute to increased risk, while maintaining a healthy weight, reducing inflammation, and consuming essential nutrients can lower it. Dr. Gorman and Texas Breast Center team recommend a balanced diet with fruits, vegetables, whole grains, lean proteins, and healthy fats, limiting processed foods, sugary and alcoholic beverages, and excessive red or processed meat. Research suggests a Mediterranean diet and possibly a high soy diet, combined with regular physical activity and limited alcohol consumption, is the most effective approach, although the evidence on soy is mixed. In summary, a nutrient-dense diet can lower breast cancer risk and improve overall health. Dr. Gorman and her team are dedicated to helping patients make informed dietary choices and develop healthy eating habits for long-term breast health and overall well-being.
Obesity
Obesity, particularly after menopause, is a significant breast cancer risk factor, linked to increased estrogen production, insulin levels, and poorer prognosis for diagnosed individuals. Dr. Gorman of Texas Breast Center emphasizes the importance of healthy weight management through a balanced diet, regular physical activity, and behavioral changes, promoting a gradual weight loss of 0.5 to 1 kg per week. She provides personalized support for her patients to develop a sustainable plan, set realistic goals, and seek necessary support, as it is not only about reducing breast cancer risk but also promoting overall well-being. In summary, maintaining a healthy weight can lower breast cancer risk, and Dr. Gorman and her team are committed to supporting their patients in managing their weight and reducing their breast cancer risk.
Smoking
Long-term smoking is linked to a modest increase in breast cancer risk, especially in premenopausal women, and various other health risks, such as lung cancer, cardiovascular disease, and stroke. Dr. Gorman and Texas Breast Center team advise against smoking and provide support and resources for those wishing to quit. Although the breast cancer risk associated with smoking is modest compared to obesity or family history, quitting smoking improves overall health. Passive smoking may also increase breast cancer risk, so avoiding secondhand smoke is advised. Dr. Gorman is committed to supporting patients in their journey to quit smoking. In summary, quitting smoking is crucial for reducing breast cancer risk and promoting overall health, and Texas Breast Center team is dedicated to helping patients quit smoking and improve their well-being.
Night Shift Work
Night shift work can disrupt circadian rhythms and melatonin production, potentially increasing breast cancer risk, although evidence is not entirely consistent. Dr. Gorman at Texas Breast Center advises patients to practice good sleep hygiene, including a regular sleep schedule and minimizing screen exposure before bedtime, and for those working night shifts, wearing blue light-blocking glasses and maintaining a regular sleep schedule on days off. While the increase in risk is modest compared to other factors like obesity or family history, it is a modifiable risk factor worth considering. In summary, practicing good sleep hygiene and minimizing artificial light exposure at night can help reduce breast cancer risk. Dr. Gorman and her team provide personalized recommendations and support to manage breast cancer risk and promote overall well-being.
Maintaining a Healthy Weight
Maintaining a healthy weight is vital for reducing breast cancer risk, particularly postmenopausal women, as obesity increases estrogen and insulin levels, both linked to higher breast cancer risk. Dr. Gorman and her team at Texas Breast Center offer personalized support for lifestyle changes like a healthy diet and regular physical activity. While BMI is a common measure of healthy weight, it doesn’t consider muscle mass, bone density, or body composition. Overall, a healthy weight reduces breast cancer risk and benefits overall health. Dr. Gorman’s team provides personalized recommendations to help patients maintain a healthy weight and improve their well-being.
Take Control of Your Health Today!
Breast cancer risk is influenced by several factors, including obesity, night shift work, smoking, physical inactivity, poor diet, and unhealthy body weight. Dr. Gorman and her team at Texas Breast Center are dedicated to helping patients manage these modifiable risk factors through personalized recommendations and support. Achieving a healthy weight, engaging in regular physical activity, consuming a balanced diet, avoiding smoking and excessive alcohol consumption, and managing exposure to artificial light at night can all contribute to reducing breast cancer risk and promoting overall health and well-being.
Take control of your health today by making positive lifestyle changes that can reduce your risk of breast cancer and improve your overall well-being. Schedule an appointment with Dr. Gorman and her team at Texas Breast Center to receive personalized recommendations and support tailored to your unique needs and circumstances. Remember, a healthier you is possible, and it starts with taking the first step towards a brighter, healthier future. Act now to take control of your health and reduce your breast cancer risk!
See the other articles in the Causes series, including Genetic Mutations and Gender Influencing Causes.
Frequently Asked Questions About Breast Cancer Causes: Lifestyle Risks
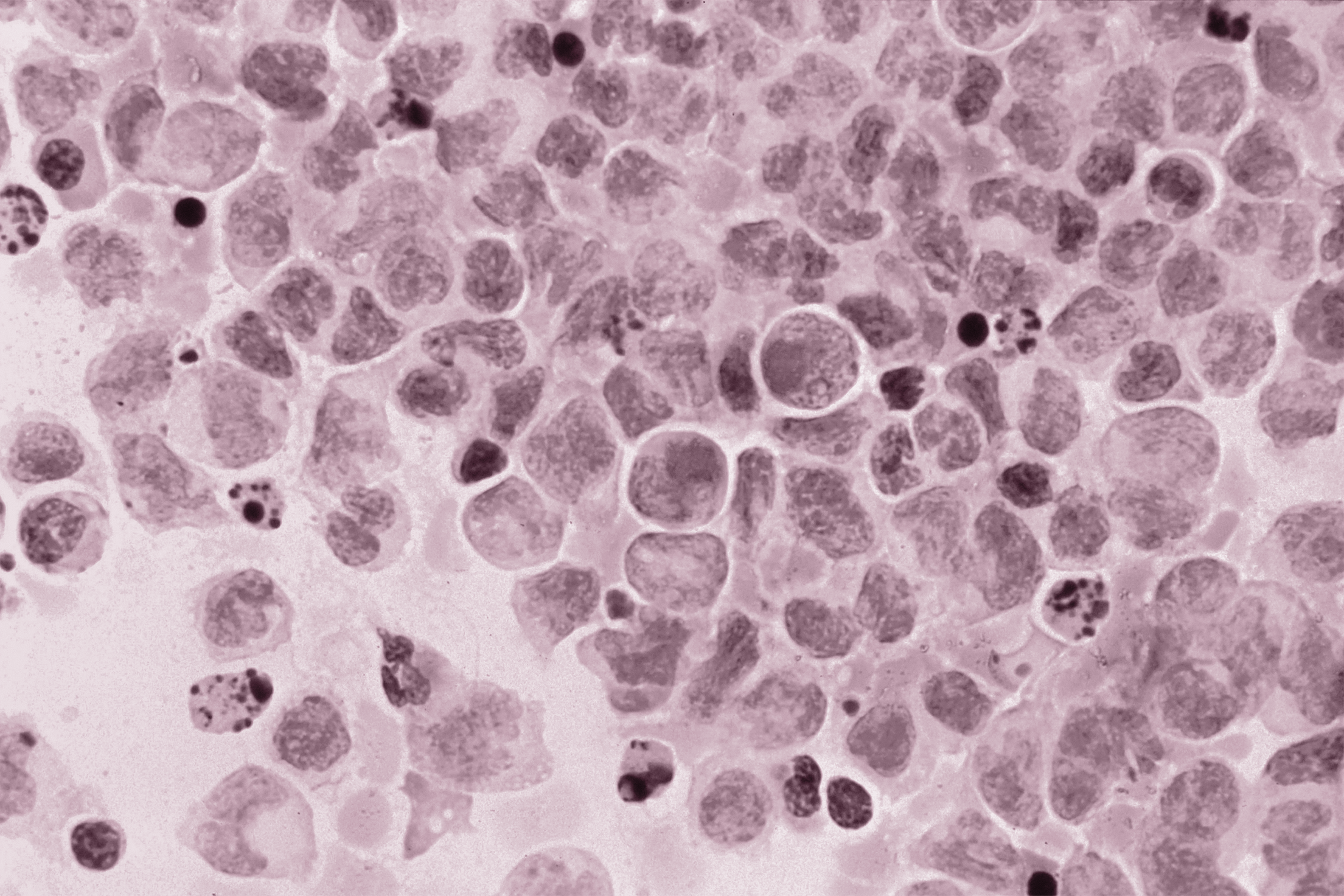
What types of breast cancer are most common, and how does weight gain affect my risk?
There are several types of breast cancer, but the most common ones are ductal carcinoma in situ (DCIS), invasive ductal carcinoma, and invasive lobular carcinoma. Weight gain, especially after menopause, increases the risk of breast cancer due to higher estrogen production in fat tissue. Maintaining a healthy body weight is crucial for reducing the risk of breast cancer and other health issues. At Texas Breast Center, we provide personalized support and recommendations to help our patients maintain a healthy weight and reduce their breast cancer risk.
How does hormone therapy and hormone replacement therapy affect breast cancer risk?
Hormone therapy, specifically menopausal hormone therapy (MHT) and hormone replacement therapy (HRT), is associated with an increased risk of breast cancer. Combined oral contraceptive pills, which contain estrogen and progestin, also slightly increase the risk of breast cancer. However, the risk decreases over time once these medications are stopped. It’s important to discuss the risks and benefits of hormone therapy with your healthcare provider. At Texas Breast Center, we provide personalized recommendations to help our patients make informed decisions about their health.
Does drinking alcohol or smoking increase my risk for breast cancer?
Yes, drinking alcohol and smoking are both associated with an increased risk of breast cancer. The risk increases with the amount of alcohol consumed and the duration of smoking. It is advisable to limit alcohol consumption to moderate levels or avoid it altogether and to quit smoking. At Texas Breast Center, we provide resources and support for those who wish to quit smoking and limit alcohol consumption.
Is there a link between breast density and breast cancer?
Yes, having dense breast tissue is a known risk factor for breast cancer. Dense breast tissue can make it harder for mammograms to detect breast cancer, and women with dense breasts may need additional screening tests. It is important to discuss your breast density and what it means for your screening guidelines with your healthcare provider. At Texas Breast Center, we provide personalized screening recommendations based on each patient’s unique needs and circumstances.
What are the signs and symptoms of breast cancer?
Common signs and symptoms of breast cancer include a lump in the breast or underarm, changes in the size, shape, or appearance of the breast, unexplained pain in the breast or nipple, nipple discharge, and skin changes on the breast. However, it is important to note that many breast conditions that cause similar symptoms are not cancerous. Early detection is crucial for successful treatment, so it is important to have regular breast cancer screenings and to consult a healthcare professional if you notice any unusual changes in your breasts. At Texas Breast Center, we are committed to providing comprehensive breast health care, including screening, diagnosis, and treatment.
What is the role of genetics and BRCA mutation in breast cancer?
Genetics play a significant role in breast cancer risk. Specific genetic mutations, such as BRCA1 and BRCA2, significantly increase the risk of developing breast and ovarian cancer. It is important to discuss your family history of cancer and consider genetic testing if you have a strong family history of breast or ovarian cancer. At Texas Breast Center, we provide genetic counseling and testing to help our patients understand their risk and make informed decisions about their health.
Can physical activity and diet reduce the risk of breast cancer?
Yes, regular physical activity and a healthy diet can reduce the risk of breast cancer. The American Cancer Society recommends at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week for cancer prevention. A diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats can also contribute to lower breast cancer risk and improve overall health. At Texas Breast Center, we provide personalized recommendations and support to help our patients incorporate regular physical activity and a healthy diet into their daily routine.
Is breast cancer screening necessary for all women?
Breast cancer screening is important for all women, but the screening guidelines may vary based on individual risk factors such as age, family history, and breast density. Regular mammograms are recommended for women starting at age 40 or 50, depending on individual risk factors. It is important to discuss your personal risk factors and screening recommendations with your healthcare provider. Texas Breast Center provides personalized screening recommendations based on each patient’s unique needs and circumstances.
What are the options for breast reconstruction surgery after mastectomy?
Breast reconstruction surgery can be done using several different methods, including implants, tissue flaps, or a combination of both. The best method for you will depend on your individual circumstances, including your overall health, the size and shape of your breasts, and your personal preferences. It is important to discuss your options and the potential risks and benefits of each method with your healthcare provider. At Texas Breast Center, we provide personalized recommendations and support to help our patients make informed decisions about their breast reconstruction options.
How does being overweight or obese impact my risk of developing breast cancer?
Being overweight or obese is associated with increased levels of estrogen and insulin in the body, which can elevate the risk of breast and endometrial cancer. Excess fatty tissue increases estrogen production, which is a known risk factor for breast cancer, especially in postmenopausal women. The Texas Breast Center can help with personalized recommendations for maintaining a healthy weight and reducing cancer risk.
Can oral contraceptives or hormone replacement therapy increase my risk of breast cancer?
Yes, using oral contraceptives or postmenopausal hormone therapy, especially those containing both estrogen and progestin, can slightly increase the risk of developing breast cancer. Bioidentical hormone therapy and contemporary hormonal contraception have similar risks. It’s essential to discuss your personal history and risk factors with your healthcare provider at the Texas Breast Center before starting any hormone therapy or birth control medicine.
How does smoking and alcohol consumption affect my breast cancer risk?
Exposure to cigarette smoke and drinking alcohol increases the risk of developing breast cancer. Alcohol raises estrogen levels in the body, while toxins in cigarette smoke can damage DNA in breast cells, leading to invasive cancer. The Texas Breast Center recommends smoking cessation, limiting alcohol intake, and adopting a healthy lifestyle to reduce your risk.
Does my diet play a role in breast cancer prevention?
Absolutely. A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and low in processed foods, sugary beverages, and red meat can contribute to breast cancer prevention. Some studies suggest that a plant-based whole food diet, high in soy products, and low in western dietary pattern foods can reduce breast cancer risk. However, the evidence on soy products is mixed, and more research is needed. The Texas Breast Center provides personalized dietary recommendations and support to help you maintain a healthy diet and reduce your breast cancer risk.
How can I modify my breast cancer risk, and does pregnancy or breastfeeding affect my risk?
Being physically active, maintaining a healthy weight, and practicing mindfulness-based stress reduction can help modify breast cancer risk. Pregnancy and breastfeeding can lower your risk, as can limiting exposure to estrogen therapy and hormone replacement therapy. Having a child before age 30 and breastfeeding for at least six months can also reduce risk. At the Texas Breast Center, we provide comprehensive advice and support to help you understand and manage all known risk factors for breast cancer.
How does having a BRCA1 or BRCA2 mutation affect my breast cancer risk?
Having a BRCA1 or BRCA2 mutation significantly increases a person’s risk of developing breast and ovarian cancer. Regular screening mammograms, clinical oncology consultations, and preventive healthcare measures, such as risk-reducing surgeries (e.g., having your ovaries removed), are essential for individuals with these genetic mutations. The Texas Breast Center provides personalized care and support for individuals with BRCA1 or BRCA2 mutations to help manage their increased risk.
Does taking certain medications like aromatase inhibitors or letrozole affect my breast cancer risk?
Aromatase inhibitors and letrozole are medications used to reduce the risk of breast cancer recurrence in postmenopausal women with hormone receptor-positive breast cancer. While these medications can reduce the risk of breast cancer recurrence, they can have side effects such as symptoms of menopause, edema, and bone loss. It’s essential to discuss the benefits and risks of these medications with your healthcare provider at the Texas Breast Center.

 Late in 2017, the media picked up on a
Late in 2017, the media picked up on a