 Cancer is perhaps the scariest word in the dictionary, capable of striking fear into the heart of anyone who hears it inside of a second. Part of the problem is that the minute a doctor says that word, anything that he or she says subsequently becomes a total blur. It is like the patient is trying to listen to the doctor while being underwater. That’s the reason we have a resource section on our site. This article answers questions about the procedure for a biopsy of the sentinel lymph node.
Cancer is perhaps the scariest word in the dictionary, capable of striking fear into the heart of anyone who hears it inside of a second. Part of the problem is that the minute a doctor says that word, anything that he or she says subsequently becomes a total blur. It is like the patient is trying to listen to the doctor while being underwater. That’s the reason we have a resource section on our site. This article answers questions about the procedure for a biopsy of the sentinel lymph node.
As a doctor, I try to provide as much explanation and support to my patients throughout the course of their treatment.
Initially, as would be expected, their knowledge of cancer and the various procedures associated with it are normally minimal. As time progresses, and the treatments begin, their knowledge grows, but when they are first trying to comprehend that they might have cancer, the more information with which I can provide them, the better.
Patients regularly tell me that they have an unquenchable thirst for information; there is, after all, nothing worse than the unknown. In fact, once they have a definitive diagnosis, they then feel empowered and more able to fight, because they know exactly what it is they are fighting.
What Is A Sentinel Lymph Node?
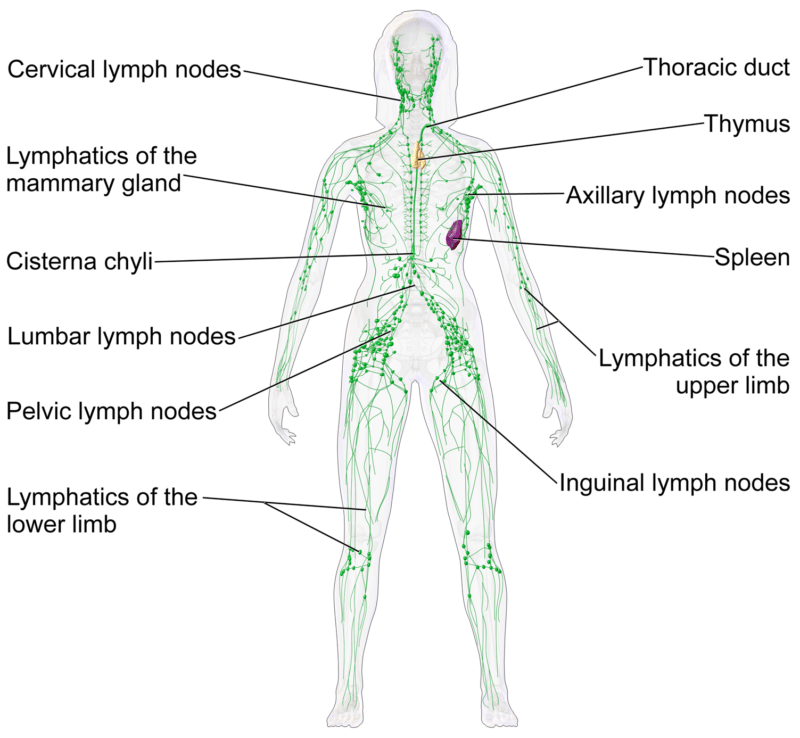
Lymph Nodes are part of the body’s immune system, and in very basic terms are a transportation network for a fluid which is called lymph. Your body’s lymph system aims to fight infection, and it does this by attacking and ultimately destroying abnormal or old cells. Most people will have experience of their lymph nodes being enlarged in the neck area when they have a bad cold, flu or throat infection.
An Illustration to Make Things Simpler
Perhaps the best way of describing how a Sentinel Node biopsy works is to imagine the lymph nodes as a set of vehicles on highway I-35.
When I perform a Sentinel Lymph Node Biopsy, I am trying to ascertain how far along the road the cancer has spread. A Sentinel Lymph Node biopsy will typically be performed at the time of the breast surgery.
By performing this test, I can see whether or not the cancer has spread outside of the breast itself, and subsequently make a decision on the most appropriate form of treatment, such as chemotherapy, dependent upon the results.
In most cases, a Sentinel Node biopsy will be the second in a series of tests. Initially, most women will be sent for an ultrasound scan of the area under the arms.
As cancer spreads throughout the body, it leaves traces of its presence, so it is critical for a doctor to be able to ascertain how far any cancer has spread.
Historically, doctors used to remove as many lymph nodes from under the arm as possible, in the belief that the more information they had about the cancer, the more successful they could be. This thinking changed with the invention of the Sentinel Lymph Node Biopsy.
If we return to our I-35 highway explanation, then it is fair to assume that every vehicle who wants to drive the entire route will start at one end or the other of the highway.
For our example, let’s assume we are staring at the southern end of the highway in Laredo, TX. If we could isolate the Austin, TX section of I-35 and identify whether or not a vehicle has passed through that section, then that could provide us with vital information.
Let’s assume that we discover that the vehicle in question has not entered Austin; if that is the case, then there is no need to check any further up the highway and check in Austin, Waco or Dallas, and the same applies to performing a Lymph Node Biopsy.
How is a Sentinel Lymph Node Biopsy Performed?
As a breast cancer surgeon, I can determine where the cancer is within the breast, and can then determine the extent of lymph node involvement using this innovative biopsy procedure.
Typically, the day of the procedure, I will inject some mildly radioactive dye into the breast close to the site of the cancer. During the procedure, I will then inject further blue dye into the breast, and then monitor the flow of that dye and the radioactive dye to determine which lymph node drains that area.
This then enables me to see which lymphatic nodes are the first in line. By a process of deduction, rather than removing a lot of lymph nodes, under Sentinel Lymph Node Biopsy procedures, I only need to remove the closest lymph nodes to the breast. If after testing these nodes the results are clear, then there is a very high level of probability that any lymph nodes further along “the highway” are clear of cancer as well.
Is A Sentinel Lymph Node Biopsy Suitable In All Cases?
Although this procedure is much less invasive and has a high level of success, there are certain situations in which a woman will not be offered this type of biopsy. The American Society Of Clinical Oncology published some guidance in 2014 as to situations where a Sentinel Lymph Node Biopsy was inappropriate. The exemptions were as follows
• Any woman who may be pregnant
• Any case where a low-grade ductal carcinoma in situ (DCIS) is being treated with a lumpectomy
• The cancer is spread outside the breast and/or lymph nodes.
Further dissection of lymph nodes is necessary when some of the sentinel lymph nodes are positive for cancer cells.
Once We Get Your Biopsy Results
It is important to remember that a Sentinel Lymph Node Biopsy is a relatively simple procedure, and should be thought of as a tool to help us make important decisions about the intensity of the treatment you require. These biopsies are valuable in helping to diagnose exactly how far the cancer has spread and can be very beneficial to both the patient and me as we determine treatment. Once the results are back, we will then have a discussion about the next steps in your treatment.

Valerie Gorman, MD, FACS, is a breast cancer surgeon. She is board certified by the American Board of Surgery and serves as Chief of Surgery and Medical Director of Surgical Services at Baylor Scott & White Medical Center – Waxahachie. She is the Clinical Assistant Professor of Medical Education position at the Texas A&M University College of Medicine.
- Certificate, Physician Leadership Program, Southern Methodist University, Dallas, Texas (2010)
- M.D., University of Texas Southwestern Medical School at Dallas, Texas (June 1999)
- B.S., Biola University, LaMirada, California, (1994) Magna Cum Laude
Major: Biochemistry - Residency in General Surgery, University of Texas Southwestern Medical Center at Dallas, Texas (June 2004)